comparing different anticoagulants, warfarin, coumadin, doacs
- related: Hemeonc
- tags: #hemeonc
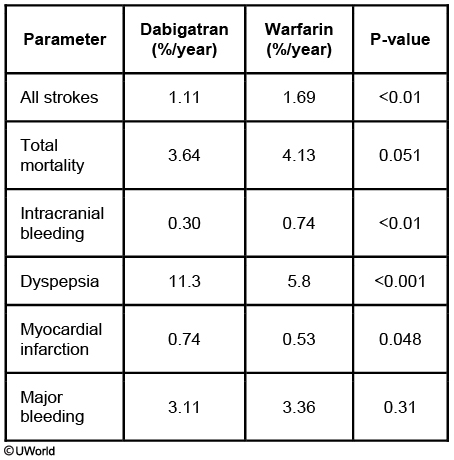
Systemic thromboembolism is a major cause of long-term morbidity in patients with atrial fibrillation. Treatment with warfarin or target-specific oral anticoagulants (TSOACs: dabigatran, rivaroxaban, apixaban, edoxaban) has been shown to significantly reduce the risk of embolization in patients at moderate to high risk for thromboembolic events. Dabigatran is an oral direct thrombin inhibitor that decreases the risk of thromboembolic events in patients with nonvalvular atrial fibrillation.
In randomized controlled trials, anticoagulation with TSOACs has shown lower rates of both ischemic stroke and major bleeding compared to warfarin. More importantly, their use is associated with a significant reduction in the risk of hemorrhagic stroke and/or intracranial bleeding, as well as all-cause mortality. However, they are not recommended for use in certain patient subsets, including:
- Patients with renal failure (CrCl <30 mL/min) or end-stage renal disease
- Patients with valvular heart disease (mitral stenosis, prosthetic heart valves, severe decompensated valvular disease likely to require valve replacement)
- Pregnant patients
Neither TSOACs nor warfarin is associated with an increased risk of pericarditis. However, anticoagulants should be used with caution in patients with pericarditis as both TSOACs and warfarin have been associated with hemorrhagic transformation.
There was a slightly increased risk of myocardial infarction in patients taking dabigatran compared to warfarin.